For this week's case, I'm going to take advantage of whole slide imaging technology via the cloud. The specimen is a section of large bowel obtained at autopsy. The prosectors were surprised to see several small worm-like objects attached to the bowel mucosa and therefore submitted representative sections for processing and microscopic examination. Here is a representative view of what they found:
To see the entire slide and zoom in on the diagnostic areas, click HERE.
Note that you don't need to download any special software to view this slide. You can use the "+" sign to zoom in, or simply use the track wheel on your mouse. It's pretty slick! Special thanks to Dr. Andy Norgan who made "Helminths in the Cloud" possible.
Monday, July 30, 2018
Sunday, July 29, 2018
Answer to Case 504
Answer: Trichuris trichiura, the human whipworm.
It's hard to top Blaine's excellent description of the diagnostic features for this case:
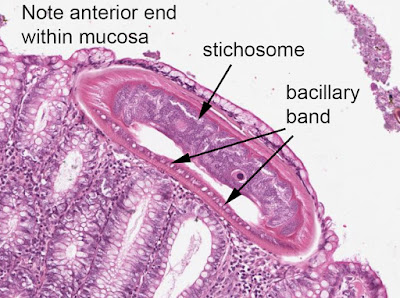
"Trichuris trichiura. If the eggs in utero were not enough, there is also stichocytes and bacillary bands (best seen in the anterior end of the worm within the tissue), polymyarian/coelomyarian musculature, and a strongly nucleated hypodermis. The size and egg morphology rules-out Capillaria philippinensis, which would also be in the intestinal tract and have trichuroid features of stichocytes and bacillary bands."
William Sears also pointed out a helpful feature: "it is telling that the thinner head part is embedded in the tissue and the larger tail is not embedded consistent with whipworm." Besides the eggs, the location in the tissue is one of the key features. Here are some of these diagnostic features:
Thanks again to everyone who wrote in, and to my Clinical Microbiology fellow, Dr. Andy Norgan, who came up with the cool programming to rapidly and nearly-seamlessly display whole-slide digital images. For those of you who couldn't get the embedded link to work for you, try this one instead:
https://s3.us-east-2.amazonaws.com/mcr-id-path/slides/BEOEOz_wVUmkRf2L2oG2sg.html
It's hard to top Blaine's excellent description of the diagnostic features for this case:
"Trichuris trichiura. If the eggs in utero were not enough, there is also stichocytes and bacillary bands (best seen in the anterior end of the worm within the tissue), polymyarian/coelomyarian musculature, and a strongly nucleated hypodermis. The size and egg morphology rules-out Capillaria philippinensis, which would also be in the intestinal tract and have trichuroid features of stichocytes and bacillary bands."
William Sears also pointed out a helpful feature: "it is telling that the thinner head part is embedded in the tissue and the larger tail is not embedded consistent with whipworm." Besides the eggs, the location in the tissue is one of the key features. Here are some of these diagnostic features:
Eggs with polar plugs (arrows; below):
As many of you may know, the whipworm gets it's name from it's shape - a skinny end and a thicker end, giving the worm a 'whip-like' shape. Unlike what is typically expected, however, the skinny end is anterior - not posterior. When my students find this puzzling, I ask them what they would rather try to do - insert the thin, needle-like end of the worm into the colonic mucosa, or the fat end? I also ask them what makes more sense - having the end with eggs hanging free in the lumen or caught up in the mucosa? This usually helps them conceptualize the worm's morphology, and I think they tend to remember it as well. When it comes to trying to remember the location in the gut, I ask my students what the dreaded complication of whipworm infection is. They always remember that it is rectal prolapse! Once they remember involvement of the rectum, it's easy for them to remember that it's the large bowel rather than the small bowel that is typically involved.
Thanks again to everyone who wrote in, and to my Clinical Microbiology fellow, Dr. Andy Norgan, who came up with the cool programming to rapidly and nearly-seamlessly display whole-slide digital images. For those of you who couldn't get the embedded link to work for you, try this one instead:
https://s3.us-east-2.amazonaws.com/mcr-id-path/slides/BEOEOz_wVUmkRf2L2oG2sg.html
Monday, July 23, 2018
Case of the Week 503
This week's case is a fun identification from Florida Fan. A podiatrist submitted a toe nail sample from an elderly female for fungal smear and culture. Fungus wasn't seen using KOH Calcofluor staining, but instead something else was noted:
Identification? And any thought on what it's doing on a toe?
Identification? And any thought on what it's doing on a toe?
Answer to Case 503
Answer: Demodex folliculorum, the follicle mite.
What is it doing on the toe? Well, toes have follicles too! It's true that we generally think of these little mites on the face, but they can be found anywhere on the skin. Interestingly, dogs (and possibly other animals) can get severe infection of their paws from Demodex species (called demodectic mange). In humans, Demodex are mostly considered to be harmless inhabitants of our skin.
Here is a nice side-by-side view of the 2 images in this case:
Note the presence of 8 legs in the adult form (mites are arachnids and not insects). Thanks again to Florida Fan for these lovely images!
What is it doing on the toe? Well, toes have follicles too! It's true that we generally think of these little mites on the face, but they can be found anywhere on the skin. Interestingly, dogs (and possibly other animals) can get severe infection of their paws from Demodex species (called demodectic mange). In humans, Demodex are mostly considered to be harmless inhabitants of our skin.
Here is a nice side-by-side view of the 2 images in this case:
Note the presence of 8 legs in the adult form (mites are arachnids and not insects). Thanks again to Florida Fan for these lovely images!
Monday, July 16, 2018
Case of the Week 502
This week's case is of a patient with recurrent fevers. No further history is available, but the following were noted on Giemsa-stained thin blood films:
Identification? What additional test would be helpful for confirming your diagnosis?
Identification? What additional test would be helpful for confirming your diagnosis?
Sunday, July 15, 2018
Answer to Case 502
Answer: Borrelia spp., relapsing fever group. Molecular studies are needed to definitively identify the causative agent. However, knowing the exposure history of the patient also helps narrow the differential. In this case, we later found out that the patient is from the northwestern part of North America, and therefore this is most likely Borrelia hermsii, one of the tick-borne relapsing fever Borrelia species. The other tick-borne Borrelia in North America are B. parkerii and B. turicatae. These species are transmitted through the bite of a soft-bodied tick in the genus Ornithodoros, and are usually associated with exposure to 'rustic' settings such as cabins and lean-tos. There is a nice article on the geographic distribution of B. hermsii that you can read HERE.
Borrelia recurrentis, the causative agent of louse-borne relapsing fever, is rarely seen in North America, given that body lice are relatively uncommon and usually associated with overcrowding and social disruption. However, B. recurrentis infection has a similar clinical presentation to the tick-borne relapsing fevers, and the spirochetes have an identical appearance on peripheral blood smear.
Borrelia spirochetes appear as long spiral-shaped bacilli (5-20 microns in length) with relatively regular undulations. As William mentions, there are other spiral-shaped or curved bacteria as well; some are curved or wavy rods (e.g. Vibrio, Campylobacter, Helicobacter), whereas others are true spirochetes (Borrelia, Treponema and Leptospira spp.). Of the true spirochetes, only the relapsing fever Borrelia are regularly seen in blood. Therefore, this thin blood film appearance in conjunction with the clinical history of recurrent (i.e. relapsing) fevers is consistent with tick-borne relapsing fever.
As Blaine and Idzi mention, Borrelia burgdorferi, the primary cause of Lyme disease in North America, does NOT reach sufficient levels in blood to be seen on peripheral blood smear (mean number of spirochetes is 0.1 per mL of blood). Having said that, some mentioned that the newly-described Borrelia mayonii HAS been noted to have high levels of bacteremia in peripheral blood, and therefore could potentially be seen on peripheral blood smear. Good catch! While spirochetes of Borrelia mayonii may be seen on peripheral blood smears, they are in relatively low numbers - ~2 spirochetes per 70 high power fields - so while visible, they would not be in such abundance as seen in this case.
Finally, some of you may be wondering why I've included a bacterial case on this blog devoted to parasites. The reason is that parasitologists can play an important role in identifying other microorganisms when seen on conventional parasitology preparations such as thin blood films. Borrelia spirochetes, Ehrlichia/Anaplasma morulae, and intracellular yeasts (e.g. Histoplasma capsulatum) are the more common non-parasites that can be seen on blood smears, and therefore it's helpful to be familiar with their appearance. We've seen all 3 in just the past year! Here are links to 2 past cases:
Case of the Week 165: Anaplasma phagocytophilum morulae within neutrophils
Case of the Week 492: Histoplasma capsulatum within phagocytic cells
Borrelia recurrentis, the causative agent of louse-borne relapsing fever, is rarely seen in North America, given that body lice are relatively uncommon and usually associated with overcrowding and social disruption. However, B. recurrentis infection has a similar clinical presentation to the tick-borne relapsing fevers, and the spirochetes have an identical appearance on peripheral blood smear.
Borrelia spirochetes appear as long spiral-shaped bacilli (5-20 microns in length) with relatively regular undulations. As William mentions, there are other spiral-shaped or curved bacteria as well; some are curved or wavy rods (e.g. Vibrio, Campylobacter, Helicobacter), whereas others are true spirochetes (Borrelia, Treponema and Leptospira spp.). Of the true spirochetes, only the relapsing fever Borrelia are regularly seen in blood. Therefore, this thin blood film appearance in conjunction with the clinical history of recurrent (i.e. relapsing) fevers is consistent with tick-borne relapsing fever.
As Blaine and Idzi mention, Borrelia burgdorferi, the primary cause of Lyme disease in North America, does NOT reach sufficient levels in blood to be seen on peripheral blood smear (mean number of spirochetes is 0.1 per mL of blood). Having said that, some mentioned that the newly-described Borrelia mayonii HAS been noted to have high levels of bacteremia in peripheral blood, and therefore could potentially be seen on peripheral blood smear. Good catch! While spirochetes of Borrelia mayonii may be seen on peripheral blood smears, they are in relatively low numbers - ~2 spirochetes per 70 high power fields - so while visible, they would not be in such abundance as seen in this case.
Finally, some of you may be wondering why I've included a bacterial case on this blog devoted to parasites. The reason is that parasitologists can play an important role in identifying other microorganisms when seen on conventional parasitology preparations such as thin blood films. Borrelia spirochetes, Ehrlichia/Anaplasma morulae, and intracellular yeasts (e.g. Histoplasma capsulatum) are the more common non-parasites that can be seen on blood smears, and therefore it's helpful to be familiar with their appearance. We've seen all 3 in just the past year! Here are links to 2 past cases:
Case of the Week 165: Anaplasma phagocytophilum morulae within neutrophils
Case of the Week 492: Histoplasma capsulatum within phagocytic cells
Tuesday, July 10, 2018
Case of the Week 501
This week's case features a zoonotic infection that can potentially involve humans. The patient is a sheep named Mr. Grumpy. Although grumpiness is his usual state of being, he was particularly grumpy when I saw him because he had a wound infested with maggots. Wounds in sheep can be difficult to detect early on because they are often hidden under dense wool. Poor Mr. Grumpy had likely acquired his wound while in a new pasture, and it had taken several days before behavior changes alerted the owners to his condition.
Here is the original photo of his wound (warning - not for the squeamish), followed by one after he has been shorn and cleaned up a bit:
Many thanks to Terri who allowed me to participate in removing the maggots from Mr. Grumpy and make him (hopefully) less grumpy. Harry (my student from London) and I plucked them one at a time from the wound and placed them in 70% ethanol for transport to the lab:
Here is a close up of the wool above the wound where a lot of the maggots were hiding:
Here they are some that were removed from the deep wound:
Once we were back in the lab, this is what we saw:
What is the identification of these maggots?
Here he is today - doing much better!
Here is the original photo of his wound (warning - not for the squeamish), followed by one after he has been shorn and cleaned up a bit:
Many thanks to Terri who allowed me to participate in removing the maggots from Mr. Grumpy and make him (hopefully) less grumpy. Harry (my student from London) and I plucked them one at a time from the wound and placed them in 70% ethanol for transport to the lab:
Here they are some that were removed from the deep wound:
Once we were back in the lab, this is what we saw:
What is the identification of these maggots?
Here he is today - doing much better!
Sunday, July 8, 2018
Answer to Case 501
Answer: blow fly larvae; either Phormyia regina (black blow fly) or Cochliomyia macellaria (secondary screwworm)
This was a tricky one given the somewhat overlapping features of these two species' third instar larvae. If you follow the CDC's pictorial key, you get to the following branch point where you have to decide if:
1. There is a clearly visible button
2. The walls of the slits have lateral swellings
Having examined the maggots myself, I can say that the button is present, but not very distinct, and I believe I see faint lateral swellings on the slides. Therefore, my interpretation is that this is Cochliomyia macellaria. Here is my best attempt to capture these diagnostic features:
There is little clinical difference between P. regina and C. macellaria. Both can colonize the wounds of livestock and humans and feed on dead tissue. Fortunately neither feed on living tissue and therefore don't pose the same risk to livestock as the primary screwworm, Cochliomyia hominivorax, which has been eliminated from the United States using a sterile fly release program. Of note, C. hominivorax recently made a comeback in the Florida keys, necessitating a renewed sterile fly release program to eliminate the population. The University of Florida Entomology and Nematodology Department has a nice educational piece on the primary screwworm that you can read HERE.
Thanks to all of my entomology-minded colleagues who took the time to write in on this post!
This was a tricky one given the somewhat overlapping features of these two species' third instar larvae. If you follow the CDC's pictorial key, you get to the following branch point where you have to decide if:
1. There is a clearly visible button
2. The walls of the slits have lateral swellings
Having examined the maggots myself, I can say that the button is present, but not very distinct, and I believe I see faint lateral swellings on the slides. Therefore, my interpretation is that this is Cochliomyia macellaria. Here is my best attempt to capture these diagnostic features:
There is little clinical difference between P. regina and C. macellaria. Both can colonize the wounds of livestock and humans and feed on dead tissue. Fortunately neither feed on living tissue and therefore don't pose the same risk to livestock as the primary screwworm, Cochliomyia hominivorax, which has been eliminated from the United States using a sterile fly release program. Of note, C. hominivorax recently made a comeback in the Florida keys, necessitating a renewed sterile fly release program to eliminate the population. The University of Florida Entomology and Nematodology Department has a nice educational piece on the primary screwworm that you can read HERE.
Thanks to all of my entomology-minded colleagues who took the time to write in on this post!
Monday, July 2, 2018
Case of the Week 500!!!
Welcome to my 500th Parasite Case of the Week - a special celebration of our parasitology community.
I feel so fortunate to have such wonderful readers. You keep me on my toes, send me amazing cases, and teach me a lot. I had asked for submissions of your parasite-related artwork and received some amazing entries. I put the names of all contributors into a hat and randomly selected the following 3 names:
Sheldon Campbell
Piotr Kochan
Melanie Riblett
Congratulations! I will reach out to you later to give you your prizes :)
So now without further ado, here are all of the fabulous parasite creations of our talented group:
Kate Grannis - chalk art
Marc Courturier - baked goods
Blaine Mathison - Halloween cupcakes! AND pinworm eggs - a giant scotch tape prep:

 Andrea Dahl - multimedia ticks!
Andrea Dahl - multimedia ticks!
Melissa Blessing - Giant Microbe® ghostie and bandit
Heather Rose and family - Ixodes scapularis adults and larva

Mark Fox - ink drawing of Haemonchus contortus
Alexandra Bryson - Loa loa costume
Kelly Hedlund (submitted by Ryal Relich) - Trypanosoma cruzi crochet art
The Winters - Clonorchis and snail host costumes
Piotr Kochan - photography, Ascaris and Giardia
Idzi Potters - photography
'nebula' stool crystal
Toxocara cati adult worm
Tunga penetrans
Tunga party!
Melanie Riblett - Easter eggs!
Frances Dodge - photography
And finally, from Sheldon Campbell, the fabulous singing microbiologist:
Click HERE to hear Sheldon live!
Lyrics:
Home in the Gut
Where the worms play in cheerful delight
Where the ova are shed, and the larvae are bred
And the pinworms crawl out in the night
Chorus
Where the worms play in cheerful delight
Where the ova are shed, and the larvae are bred
And the pinworms crawl out in the night
Chorus
Chorus
Chorus
Chorus
I feel so fortunate to have such wonderful readers. You keep me on my toes, send me amazing cases, and teach me a lot. I had asked for submissions of your parasite-related artwork and received some amazing entries. I put the names of all contributors into a hat and randomly selected the following 3 names:
Sheldon Campbell
Piotr Kochan
Melanie Riblett
Congratulations! I will reach out to you later to give you your prizes :)
So now without further ado, here are all of the fabulous parasite creations of our talented group:
Kate Grannis - chalk art
Marc Courturier - baked goods
Blaine Mathison - Halloween cupcakes! AND pinworm eggs - a giant scotch tape prep:

 Andrea Dahl - multimedia ticks!
Andrea Dahl - multimedia ticks!Melissa Blessing - Giant Microbe® ghostie and bandit
Heather Rose and family - Ixodes scapularis adults and larva

Mark Fox - ink drawing of Haemonchus contortus
Alexandra Bryson - Loa loa costume
Kelly Hedlund (submitted by Ryal Relich) - Trypanosoma cruzi crochet art
The Winters - Clonorchis and snail host costumes
Mark Fox and Kristine - our lovely hookworm couple
Idzi Potters - photography
'nebula' stool crystal
Toxocara cati adult worm
Tunga penetrans
Tunga party!
Melanie Riblett - Easter eggs!
Frances Dodge - photography
And finally, from Sheldon Campbell, the fabulous singing microbiologist:
Click HERE to hear Sheldon live!
Lyrics:
Home in the Gut
Copyright © 2001 by Sheldon Campbell
Oh give me a home where the parasites roam
Where the worms play in cheerful delight
Where the ova are shed, and the larvae are bred
And the pinworms crawl out in the night
Chorus
Home, home in the gut
Where the worms play in cheerful delight
Where the ova are shed, and the larvae are bred
And the pinworms crawl out in the night
Oh hookworm am I, my ova go by
In your stool and then hatch in the mud
They punch through your skin, and migrate again
To the gut, where they suck out your blood
Chorus
I live in the stream of the bile that's green
I'm Clonorchis, so please get it right
And my life's greatest wish is to enter a fish
And then you with your sushi tonight
And then you with your sushi tonight
Chorus
I cling to the wall, a tapeworm so tall
Borne by pork I came to this new home
Now while I procreate, you've got a sure date
'Cause with me you are never alone
Chorus
Please come swim with me, so that we can be free
To burrow into your bare legs
We just copulate, so we can populate
We just copulate, so we can populate
Your liver with our extra eggs
Chorus
The rectum’s my home, but I would love to roam
And lay my eggs out on your butt
I know it’s a bitch, but when you scratch that itch
My kids get into your kid’s gut.
Subscribe to:
Comments (Atom)