Answer: fly larvae from the environment, or as Florida Fan said, "agarmyiasis!"
These larvae could have originated from a number of places, including the patient's body, the blood culture bottle, the Mueller-Hinton (M-H) agar (prior to inoculation), and finally, the M-H plate inoculated with patient specimen and growing mixed bacterial and yeast colonies. However, we were able to take a logical approach to narrow the source down to one of TWO options that we felt were most likely - either the uninoculated M-H agar plate, or the plate after it was inoculated with patient specimen. We did NOT think that they came from the patient or the blood culture bottle.
Here are the factors that we considered in this assessment:
1.
The patient: As the Old One mentioned, pleural myiasis has been documented in humans - usually in the tropics in unsanitary conditions - but the shape and early instar stage of the larvae are not consistent with your typical robust bot flies, there was no cancerous mass, and, most importantly, the patient's history was NOT supportive of this diagnosis.
The lab also went back to the original blood culture bottle into which the pleural fluid had been inoculated and confirmed that no other larvae were present - thus also supporting that the pleural fluid was not the source of the larvae. To be on the safe side, more of the fluid from the blood culture bottle was inoculated onto a new agar plate and checked them for larvae; none were seen.
2.
The blood culture bottle media: this was another possibility, given that the liquid nutrient media in the blood culture bottles could potentially support the growth of fly larvae. Liquid media is made in large batches by the manufacturer and then used to make numerous bottles at once. Thus, we would have possibly seen larvae in other bottles from this same lot of media and the resultant cultures. This was not the case, suggesting that the media was not the source of contamination. Also, as mentioned above, no larvae were seen
within the blood culture bottle associated with this case.
3.
The Mueller Hinton agar: This was an intriguing possibility given that some agar plates are made by the lab. In this process, the agar is heated to liquid consistency and poured into Petri dishes on the bench top. As Florida Fan mentioned, the lids are left ajar while the agar cools to prevent condensation, during which time a fly could oviposit onto the nice warm agar. HOWEVER, the agar in this case was NOT made by the lab, but instead purchased from a commercial source. The plates were received sealed in a plastic sleeve, and were kept refrigerated until needed. Before inoculation with patient specimen, plates are allowed to come to room temperature with their lids closed. The plates are then inoculated inside of a biosafety cabinet (hopefully without flies!) and closed again. All inoculated plates are placed with their lids on within a closed incubator - again, hopefully keeping flies out.
So could have the contamination
occurred at the manufacturer, with the eggs remaining dormant on the refrigerated plates until they were inoculated and incubated? It's definitely plausible! If the
adult fly only laid eggs on a single plate, then we wouldn't expect to see contamination of other plates in this batch (again, we checked other plates from this lot of media, and no additional larvae were seen).
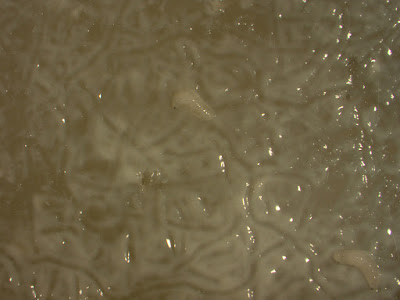
4. The agar plate with bacteria: We finally came to the M-H plate itself with its abundant growth of bacteria and yeast from the patient specimen. This was an older growth plate - 3 days - and during the time in the lab, it had been opened numerous times by multiple technologists. At 3 day, it was sitting in a bin on the bench top while the yeast was being worked up further. So could a fly have gotten in there at some point to lay eggs, and perhaps munch on the nice tasty microorganisms? This is another plausible scenario, and probably the most likely.
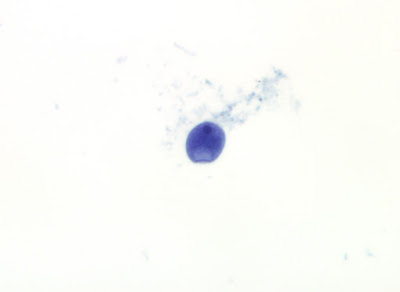
Whew! My apologies for the long explanation. Please let me know if I forget any other potential avenue for contamination. At the end of the day, the most important conclusion from this case was that the larvae did not come from the patient (who has now recovered with antimicrobial treatment) and that the source was likely environmental. We did try to identify the genus of the larvae, but they were very small (~2 mm long) and only in their second instar, thus making it difficult to provide an ID.