The following were seen in a Giemsa-stained thin blood film from a child from Cameroon.
Identification?
Monday, December 30, 2013
Sunday, December 29, 2013
Answer to Case 288
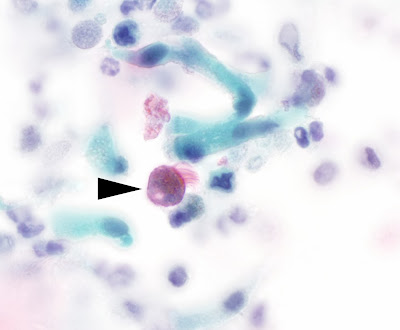
Answer: Plasmodium ovale
Marco Ligozzi and Dr. Rajani nicely described the features of P. ovale:
"The parasitized erythrocytes are oval in shape and fimbriated at the end," "Schuffner's stippling is present, more evident especially at the edges of the erythrocyte"and malaria "pigment is scattered, coarse."
Of note, Dr. Rajani points out that Schuffner's dots are "relevant to P. ovale infection; yet, these dots also appear in cases of P. vivax infection." Therefore it is incumbent upon us to look at other features that would allow us to differentiate P. ovale from P. vivax. The features that I find most useful for differentiating the 2 species are:
Here is an image from this case, demonstrating some of these important features:
Marco Ligozzi and Dr. Rajani nicely described the features of P. ovale:
"The parasitized erythrocytes are oval in shape and fimbriated at the end," "Schuffner's stippling is present, more evident especially at the edges of the erythrocyte"and malaria "pigment is scattered, coarse."
Of note, Dr. Rajani points out that Schuffner's dots are "relevant to P. ovale infection; yet, these dots also appear in cases of P. vivax infection." Therefore it is incumbent upon us to look at other features that would allow us to differentiate P. ovale from P. vivax. The features that I find most useful for differentiating the 2 species are:
- 1/3 or more of P. ovale infected erythrocytes are oval, while P. vivax infected cells are only rarely oval.
- The parasite forms of P. ovale are more compact than those of P. vivax (which are characteristically ameboid)
- Fimbriation is common with P. ovale.
- Plasmodium ovale has coarser pigment than P. vivax.
- Mature schizonts of P. ovale have 6-14 merozoites while those of P. vivax have 12-24 (obviously this feature is only helpful when you see a schizont with >14 merozoites - indicating that the species is P. vivax; immature schizonts of both species can have less than 12 merozoites, so this is less helpful).
Here is an image from this case, demonstrating some of these important features:
Monday, December 23, 2013
Sunday, December 22, 2013
Answer to Case 287
Answer: Kissing Fleas! (Ctenocephalides sp. - dog and cat flea)
From Blaine Mathison who really outdid himself on this one:
Twas the night before Christmas when all through the house
the fleas were all nestled in
the fur of the mouse.
They paired with their loved
ones under a sprig of mistletoe,
A gift from Cousin Chigoe, from
down south in the toe.
The larvae were pupating in the
bed of the host,
carrying Dipylidium
cysticercoids, an infectious dose!
The Yersinia pestis churned in
the foregut
until such time when the
proventriculus would erupt!
All of a sudden there appeared
such a clatter!
The fleas sprang from the fur to
see what was the matter.
Crawling up the leg of the host,
with such stealth and so quick,
was the holiday icon known as
St. Tick.
“Now Ixodes, now Dermacentor,
and Amblyomma!
On Rhipicephalus, Ornithodoros,
don’t forget Hyalomma.”
He got right to work and
delivered the fleas' presents
full of pathogens to spread to
medieval peasants,
Then he sprang to his sleigh and
let out a whistle,
Then they took off into the
night like a guided missile.
But I heard him exclaim as flew
out of sight,
Merry Christmas to all, and to
all a good bite!
Happy New Years Everyone!
Monday, December 16, 2013
Case of the Week 286
Sunday, December 15, 2013
Answer to Case 286
Answer: Dipylidium caninum proglottids
Although this patient is much older than usual for D. caninum infection, the appearance of these proglottids is classic, with the small size and shape resembling "grains of rice." We were also able to confirm our diagnosis by expressing immature eggs in packets out of the proglottids (1 egg packet shown by arrows below):
Although this patient is much older than usual for D. caninum infection, the appearance of these proglottids is classic, with the small size and shape resembling "grains of rice." We were also able to confirm our diagnosis by expressing immature eggs in packets out of the proglottids (1 egg packet shown by arrows below):
Monday, December 9, 2013
Case of the Week 285
This week's case was generously donated by Dr. Bryan Schmitt and Dr. Ryan Relich (Microbe Man).
An HIV positive man from the U.S. presented with multiple anal and rectal condylomas. No travel history is available. Excision with histopathology (H&E staining) showed the following:
(40x total magnification)

(500x total magnification)
(1000x total magnification)
GMS stain:
An HIV positive man from the U.S. presented with multiple anal and rectal condylomas. No travel history is available. Excision with histopathology (H&E staining) showed the following:
(40x total magnification)

(500x total magnification)
(1000x total magnification)
GMS stain:
Sunday, December 8, 2013
Answer to Case 285
Answer: leishmaniasis, presenting as atypical perianal and rectal wart-like lesions (see below for patient follow up)
As Anon and Florida Fan mention, the differential of small intracellular objects in the 2-5 micron range includes leishmania amastigotes, small yeasts (primarily Histoplasma capsulatum), microsporidia spores, and Toxoplasma gondii tachyzoites.
We can exclude Histoplasma capsulatum, other yeasts, and microsporidia based on the negative GMS stain, thereby leaving Toxoplasma and Leishmania in our differential. These two organisms are differentiated by morphologic features: Toxoplasma gondii tachyzoites are arc-shaped with a small eccentric nucleus (see case 284), while Leishmania sp. amastigotes are oval and have an eccentric nucleus AND a rod-shaped kinetoplast. Although it can be challenging to appreciate morphology in formalin-fixed, paraffin-embedded sections, this case actually allowed us to see some good examples of a kinetoplast (arrow) next to the nucleus (arrowhead):

Therefore, we can say that the patient most likely has leishmaniasis, although the unusual presentation of wart-like peri-anal and rectal lesions raises the question of whether this represents atypical cutaneous disease or visceral disease involving the GI tract and extending to the perianal skin.
To help solve this mystery, we needed additional information, and it turns out, an additional procedure needed to be performed. The patient was from Nicaragua, where cutaneous, mucocutaneous, and visceral disease has been described. He has been in the U.S. for approximately 6 years and hasn't traveled outside of the U.S. since.
To evaluate for visceral involvement, a bone marrow biopsy was then performed, which confirmed the presence of amastigotes. Therefore, this case represents an unusual presentation of visceral leishmaniasis, masquerading as anal warts!
Material from the bone marrow biopsy has now been sent to the CDC for species determination.
Many thanks to Bryan Schmitt for the interesting case!
As Anon and Florida Fan mention, the differential of small intracellular objects in the 2-5 micron range includes leishmania amastigotes, small yeasts (primarily Histoplasma capsulatum), microsporidia spores, and Toxoplasma gondii tachyzoites.
We can exclude Histoplasma capsulatum, other yeasts, and microsporidia based on the negative GMS stain, thereby leaving Toxoplasma and Leishmania in our differential. These two organisms are differentiated by morphologic features: Toxoplasma gondii tachyzoites are arc-shaped with a small eccentric nucleus (see case 284), while Leishmania sp. amastigotes are oval and have an eccentric nucleus AND a rod-shaped kinetoplast. Although it can be challenging to appreciate morphology in formalin-fixed, paraffin-embedded sections, this case actually allowed us to see some good examples of a kinetoplast (arrow) next to the nucleus (arrowhead):

Therefore, we can say that the patient most likely has leishmaniasis, although the unusual presentation of wart-like peri-anal and rectal lesions raises the question of whether this represents atypical cutaneous disease or visceral disease involving the GI tract and extending to the perianal skin.
To help solve this mystery, we needed additional information, and it turns out, an additional procedure needed to be performed. The patient was from Nicaragua, where cutaneous, mucocutaneous, and visceral disease has been described. He has been in the U.S. for approximately 6 years and hasn't traveled outside of the U.S. since.
To evaluate for visceral involvement, a bone marrow biopsy was then performed, which confirmed the presence of amastigotes. Therefore, this case represents an unusual presentation of visceral leishmaniasis, masquerading as anal warts!
Material from the bone marrow biopsy has now been sent to the CDC for species determination.
Many thanks to Bryan Schmitt for the interesting case!
Monday, December 2, 2013
Case of the Week 284
Sunday, December 1, 2013
Answer to Case 284
Answer: Toxoplasma gondii tachyzoites
Note the arc-shaped tachyzoites, each with an eccentric nucleus, amid a background of host cell nuclei.
As pointed out by Anonymous, this used to be a pretty common scenario back in the early AIDS era. Fortunately CNS toxoplasmosis is now pretty rare in the HIV positive population due to the availability of good antiretroviral medications (in parts of the world, at least) and widespread use of prophylactic medications in susceptible medications.
I don't have the full history in this patient, but there was a question about the patient's compliance with prescribed medications.
Here's a poem from Blaine this week - a little on the dark side:
Note the arc-shaped tachyzoites, each with an eccentric nucleus, amid a background of host cell nuclei.
As pointed out by Anonymous, this used to be a pretty common scenario back in the early AIDS era. Fortunately CNS toxoplasmosis is now pretty rare in the HIV positive population due to the availability of good antiretroviral medications (in parts of the world, at least) and widespread use of prophylactic medications in susceptible medications.
I don't have the full history in this patient, but there was a question about the patient's compliance with prescribed medications.
Here's a poem from Blaine this week - a little on the dark side:
Old McDonald had a
farm…E-I-E-I-O
And on his farm he had a
cat…E-I-E-I-O
With a ‘meow meow’ here and a
‘meow meow’ there…
Poopin’ out oocysts everywhere.
Necrotic cortical lesions, oh
the despair! E-I-E-I-O
Monday, November 25, 2013
Case of the Week 283
The following structures were seen on a bronchial brush specimen from an 83 year old male with a chronic cough. The structures were moving when seen in a wet prep, and there was concern from the endoscopist that these were parasites. The following photos are from the corresponding Papanicalaou stained cytology specimen.
Identification?
Identification?
Sunday, November 24, 2013
Answer to Case 283
Answer: Ciliocytophthoria, a.k.a. detached ciliary tufts from ciliated epithelial cells.
Florida Fan mentions that "Considering how many things we breath in daily, it is quite marvelous they sweep them out more efficiently than we can imagine." Very true. Our ciliated epithelial cells do an excellent job as part of the "mucociliary escalator" that removes inhaled debris from the respiratory tree. Unfortunately, various inflammatory states including asthma can cause the apical ciliated tufts of the respiratory cells to detach, and more than one investigator has mistaken these for ciliated parasites.
Of note, the only ciliated parasite of humans is Balantidium coli, a large organism (40-200 micrometers) with circumferential cilia and a classic "boring" motility. In comparison, ciliary tufts are much smaller (10-15 micrometers in diameter), have cilia arising from a flat plate-like structure, and have a beating motion in fresh preparations.
Florida Fan mentions that "Considering how many things we breath in daily, it is quite marvelous they sweep them out more efficiently than we can imagine." Very true. Our ciliated epithelial cells do an excellent job as part of the "mucociliary escalator" that removes inhaled debris from the respiratory tree. Unfortunately, various inflammatory states including asthma can cause the apical ciliated tufts of the respiratory cells to detach, and more than one investigator has mistaken these for ciliated parasites.
Of note, the only ciliated parasite of humans is Balantidium coli, a large organism (40-200 micrometers) with circumferential cilia and a classic "boring" motility. In comparison, ciliary tufts are much smaller (10-15 micrometers in diameter), have cilia arising from a flat plate-like structure, and have a beating motion in fresh preparations.
Monday, November 18, 2013
Case of the Week 282
The following is a corneal biopsy from a woman with a red and painful eye.
H&E, 100x magnification
H&E, 1000x magnification
Identification?
H&E, 100x magnification
H&E, 1000x magnification
Identification?
Sunday, November 17, 2013
Answer to Case 282
Answer: Amebic keratitis due to Acanthamoeba species. The double-walled cysts and trophozoites are characteristic:
Unfortunately this patient ended up undergoing 2 corneal transplants before she finally was cleared of infection. She now has near normal vision. Amebic keratitis can be very difficult to treat, since the presence of a single residual cyst is enough to allow for reactivation of infection after treatment or surgery.
Greater than 90% of cases in the U.S. are associated with contact lens use, as was the case with this patient.
Unfortunately this patient ended up undergoing 2 corneal transplants before she finally was cleared of infection. She now has near normal vision. Amebic keratitis can be very difficult to treat, since the presence of a single residual cyst is enough to allow for reactivation of infection after treatment or surgery.
Greater than 90% of cases in the U.S. are associated with contact lens use, as was the case with this patient.
Monday, November 11, 2013
Case of the Week 281
The following is an unstained muscle biopsy pressed between 2 glass slides. The patient experienced myalgia and facial edema 1 week after eating bear meat.
Diagnosis?
NOTE: GOOGLE + comments now disabled! (sorry about the trouble that caused for non-Google + users)
Diagnosis?
NOTE: GOOGLE + comments now disabled! (sorry about the trouble that caused for non-Google + users)
Sunday, November 10, 2013
Answer to Case 281
Answer: Trichinella species larvae.
This is the classic appearance of Trichinella larvae coiled within muscle. To answer Yenni's question, this biopsy was taken from the patient's thigh, which was quite swollen and inflamed. In autopsy specimens, good locations to look for Trichinella spp. larvae are the diaphragm and tongue.
As correctly pointed out by Anonymous, we cannot tell the species simply by looking at the larvae in biopsy, although it is possible to place the nematode in either the encapsulated group (e.g. with Trichinella spiralis) or the unencapsulated group (Trichinella pseudospiralis). A number of species have been detected from human cases in the U.S. including T. nativa, T. spiralis, and Trichinella T6.
bks asked about the risk of acquiring trichinosis from undercooked store-bought pork in the U.S. The good news is that the risk is extremely low, due to federal regulations (e.g. pigs cannot be fed uncooked meat or raw garbage) and meat inspections by the USDA. Instead, the greatest risk is from eating the meat of wild carnivores such as bear, wild pig, boar, fox and cougar. This is in marked contrast to the risk worldwide which is still due to eating pork.
To prevent trichinosis, it is best to thoroughly cook your meat (internal temperature of 160°F (71°C)). Of interest, curing and salting or freezing will kill most, but not all larvae, and some larvae are freeze-resistant. Yikes! Best to cook thoroughly, not using a microwave due to the uneven heating that may result.
This is the classic appearance of Trichinella larvae coiled within muscle. To answer Yenni's question, this biopsy was taken from the patient's thigh, which was quite swollen and inflamed. In autopsy specimens, good locations to look for Trichinella spp. larvae are the diaphragm and tongue.
bks asked about the risk of acquiring trichinosis from undercooked store-bought pork in the U.S. The good news is that the risk is extremely low, due to federal regulations (e.g. pigs cannot be fed uncooked meat or raw garbage) and meat inspections by the USDA. Instead, the greatest risk is from eating the meat of wild carnivores such as bear, wild pig, boar, fox and cougar. This is in marked contrast to the risk worldwide which is still due to eating pork.
To prevent trichinosis, it is best to thoroughly cook your meat (internal temperature of 160°F (71°C)). Of interest, curing and salting or freezing will kill most, but not all larvae, and some larvae are freeze-resistant. Yikes! Best to cook thoroughly, not using a microwave due to the uneven heating that may result.
And now a poem from Blaine Mathison, sampling RUN DMC!
This meal may send us to the
hospital
With problems musculoskeletal
It’s Trichinella all-right
Coiled in a cyst nice and tight
Lesson learned, my rhymes are
not just anecdotal
Monday, November 4, 2013
Case of the Week 280
Fluid was aspirated from 2 liver cysts in a middle aged Iraqi woman and sent to the Clinical Parasitology lab for identification. The following were seen using 400x magnification:
Identification?
Identification?
Sunday, November 3, 2013
Answer to Case 280
Answer : Echinococcus sp. protoscoleces
Thank you all for writing in. I agree that this is, statistically speaking, Echinococcus granulosus infection, although from just the microbiology findings, I would report this out as Echinococcus species, given that E. multilocularis and other Echinococcus species could have a similar presentation early on.
The key to diagnosis of echinococcosis is identification of the characteristic protoscoleces with internalized hooklets.
In the canine host, the hooklets will evert and attach to the intestinal epithelium, with subsequent development into an adult worm.
Thank you all for writing in. I agree that this is, statistically speaking, Echinococcus granulosus infection, although from just the microbiology findings, I would report this out as Echinococcus species, given that E. multilocularis and other Echinococcus species could have a similar presentation early on.
The key to diagnosis of echinococcosis is identification of the characteristic protoscoleces with internalized hooklets.
In the canine host, the hooklets will evert and attach to the intestinal epithelium, with subsequent development into an adult worm.
And now our fun poem from Blaine Mathison!
Along the banks of the Euphrates
River
An Iraqi woman started to shiver
Abdominal pain she did feel
Like a jab in the side with cold
hard steel
For she had an Echinococcus cyst
growing in her liver.
Monday, October 28, 2013
Case of the Week 279
The following ~4 mm white-cream object was identified in the diaper of a 2 year old asymptomatic male. Identification?
Subscribe to:
Comments (Atom)









































.jpg)
.jpg)
.jpg)







